The healthcare industry is changing at an incredible rate, and one of the major contributors to this change is the increasing popularity of healthcare communication through social media. Not only has social media become a place where people seek health information, but social media channels also allow for two-way public communication between patients, providers, and other third parties.
This vast network of healthcare influencers, leaders, patients, providers, organizations, and governmental entities creates a massive amount of healthcare data on a regular basis. This data, if segregated, segmented, and analyzed in a meaningful way, can offer incredible value for improving treatment efficiencies and health outcomes. This has created a demand for data aggregation and analytical tools and thus acts as an opportunity for the healthcare fraud analytics market during the forecast period.
The deployment of fraud analytics solutions is a time-consuming process. The process involves creating user interfaces, new databases, and predictive models; evaluating and deploying models, and monitoring their effectiveness. In this process, data analysts continuously run algorithms until they get the most effective predictive model.
Download PDF Brochure @ https://www.marketsandmarkets.com/pdfdownloadNew.asp?id=221837663
At times, analysts may not find the appropriate predictive model for expected outcomes, which results in time wastage. This means they must start the same process again with new data. Thus, if data analysts fail at one stage, the whole process is disturbed. Furthermore, the software requires frequent upgrades, as fraudsters constantly change tactics. This adds to the total cost of fraud analytics solutions.
The market is segmented based on solution type, delivery model, application, and end user. Based on the solution type, the descriptive analytics segment accounted for the largest share of the market in 2019. Descriptive analytics forms the base for the effective application of predictive or prescriptive analytics. Hence, these analytics use the basics of descriptive analytics and integrate them with additional sources of data in order to produce meaningful insights.
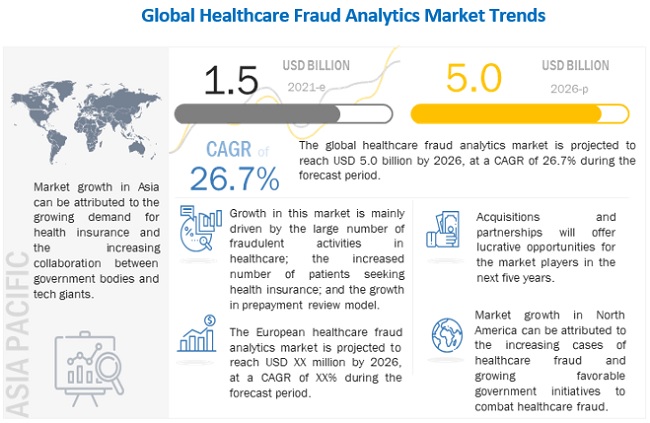
On the basis of application, the healthcare fraud analytics market is segmented into insurance claims review, pharmacy billing misuse, payment integrity, and other applications. In 2019, the insurance claims review segment dominated the global market. The increasing number of patients seeking health insurance, the rising number of fraudulent claims, and the growing adoption of the prepayment review model are expected to drive the growth of this segment in the coming years.
Geographically, the global market is segmented into North America, Europe, the Asia Pacific, Latin America, and the Middle East and Africa. North America accounted for the largest share of the global market in 2019. The high share of the North American market is attributed to the large number of people having health insurance, growing healthcare fraud, favorable government anti-fraud initiatives, the pressure to reduce healthcare costs, technological advancements.
Key Market Players
The prominent players in Healthcare Fraud Analytics Market are IBM Corporation (US), Optum, Inc. (US), Cotiviti, Inc. (US), Change Healthcare (US), Fair Isaac Corporation (US), SAS Institute Inc. (US), EXLService Holdings, Inc. (US), Wipro Limited (India), Conduent, Incorporated (US), CGI Inc. (Canada), HCL Technologies Limited (India), Qlarant, Inc. (US), DXC Technology (US), Northrop Grumman Corporation (US), LexisNexis (US), Healthcare Fraud Shield (US), Sharecare, Inc. (US), FraudLens, Inc. (US), HMS Holding Corp. (US), Codoxo (US), H20.ai (US), Pondera Solutions, Inc. (US), FRISS (The Netherlands), Multiplan (US), FraudScope (US), and OSP Labs (US).
